Lymphomatoid Granulomatosis : Morphology

Comments:
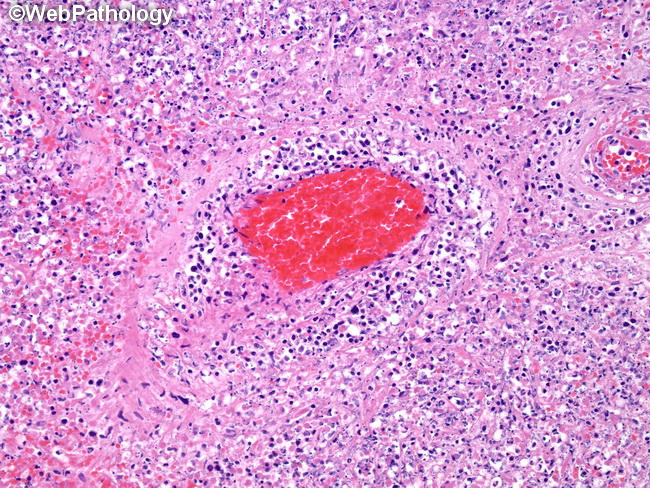
Morphology: The lymphomatoid granulomatosis lesions are characterized by angiocentric and angioinvasive lymphoid infiltrates with fibrinoid necrosis of the vessel walls and widespread necrosis of the surrounding parenchyma (as shown here). Large centrally necrotic nodules are common. There is karyorrhectic debris but no neutrophils (unlike the necrotizing lesions of Wegener's granulomatosis). The infiltrate is polymorphous and consists of small lymphocytes (mostly reactive T-cells), histiocytes, immunoblasts, and EBV-positive large atypical lymphoid cells. The number of EBV-positive cells varies within and among nodules and forms the basis of grading of LG. Cases with diffuse sheets of EBV-positive cells without an angiocentric T-cell infiltrate should be classified as EBV-positive diffuse large B-cell lymphoma. Plasma cells are not a prominent component. There are no neutrophils, eosinophils, multinucleated giant cells, or granulomas. The morphology of LG lesions in the brain, kidneys, and liver is similar to those seen in the lungs with angiocentric and angiodestructive growth pattern. In brain, it can form lymphohistiocytic nodules with necrotic centers (but no well-formed granulomas) and cause brain infarcts. The skin lesions consist of subcutaneous or dermal nodules (most common) or plaques (about 15% of cases). The lymphoid infiltrate is perivascular and periadnexal in distribution resembling lichen sclerosus et atrophicus. The infiltrate is located in the dermis and may extend into the subcutis. Granulomas are not seen. EBV-positive cells are more difficult to demonstrate than in the lungs.



