Jan 2016
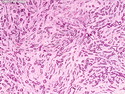
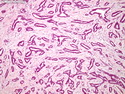
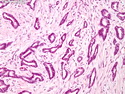
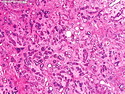
Tubular Carcinoma
Reviewer(s): Dharam M. Ramnani, MD
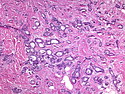
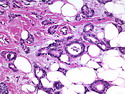
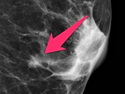
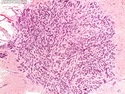
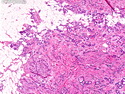
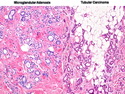
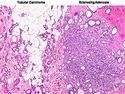
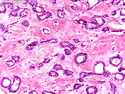
Tubular carcinoma (TCa) is a distinct subtype of invasive ductal carcinoma that is composed of simple neoplastic tubules. It makes up less than 2% of all breast cancers. The tumor size is less than 2 cm in more than 95% of cases. Most cases are non-palpable and almost always detected on screening mammography. There is a high incidence of multicentricity (56%), bilaterality (38%) and family history (40%) associated with TCa. TCa tend to be stellate or irregular lesions with infiltrating borders. There is an irregular proliferation of small glands and tubules lined by a single layer of cuboidal or columnar epithelium. At least 90% or more of the lesion should have this architecture to be classified as tubular carcinoma. The glands and tubules have angulated contours and widely open lumens. The neoplastic epithelium is homogenous and lacks significant atypia. Perineural invasion and lymphovascular invasion is rarely seen. The tubules are separated by abundant stroma containing myofibroblasts, elastic tissue, and myxoid matrix. Microcalcifications are present in about 50% of cases. Low-grade DCIS (micropapillary and cribriform type) as well as columnar cell hyperplasia with atypia (flat epithelial atypia) are considered to be the precursor lesions and are found in two-thirds of cases of TCa. ER and PR are usually positive whereas HER2/neu is negative. More than 90% of women with TCa present at Stage I. The frequency of axillary lymph node metastases is about 10%. The metastatic deposits sometimes mimic benign glandular inclusions such as endosalpingosis. The treatment usually consists of breast-conserving surgery followed by adjuvant radiation therapy. When the diagnostic criteria are applied strictly to tumors consisting entirely or almost entirely of tubular elements, the prognosis is excellent.